Introduction
Joint Effusion is more commonly known as “Water on the Knee” as it mostly affects knee joints. In layman’s terms, it’s a buildup of fluid in your joint space. The most common cause of Joint Effusion is Arthritis.
Arthritis actually affects a massive amount of people. Over 50 million adults are diagnosed with Arthritis[1] and it is the number 1 cause of disability in the USA. Since so many people suffer from Arthritis and are at high risk of getting Joint Effusion, we think it’s important you know all you can about it.
So let’s take a proper look at everything you need to know about joint effusion.
People also ask
Q. What vitamins are good for arthritis pain?
A. Nutritional deficiencies are common in arthritis sufferers which are why doctors often recommend their arthritis patient to take dietary supplements containing these nutrients to ease joint pain.. https://www.jointhealthmagazine.com/vitamins-for-arthritis-joint-pain.html
Q. What is Turmeric Curcumin Plus?
A. Turmeric Curcumin Plus is a natural dietary supplement, formulated to aid in boosting joint health and function. Its formulated from Turmeric, which is Super food and it functions well in boosting the general health and wellness of the consumer. https://www.jointhealthmagazine.com/turmeric-plus-review.html
Q. What supplement works best for joint pain?
A. Some consequences of aging – those grey hairs and crow’s feet, for instance – merely change the way we look. As we age on the outside, our joints and ligaments also get older, which often leads to joint pain. And unlike changes to our skin and hair..https://www.jointhealthmagazine.com/jointrelief
Q. How much glucosamine do I need?
A. Arthritis is a very common problem among the Americans. According to the statistics, around 22.7% of the American adults are diagnosed with some forms of arthritis, such as gout, lupus, rheumatoid arthritis, and others..https://www.jointhealthmagazine.com/whats-the-best-glucosamine-dont-take-the-wrong-kind.html
Q. What is the main cause of arthritis?
A. Arthritis is a condition that affects the body’s musculoskeletal system, mainly the joints. It’s reported that this condition is the main reason for disability among people over the age of 55 in the western countries..https://www.jointhealthmagazine.com/causes-of-arthritis.html
Q. What are the side effects of taking Omega XL?
A. Omega XL is a dietary supplement that is designed to help people with painful joints. The products is advertised as a natural supplement that uses handpicked ingredients. According to the producers..https://www.jointhealthmagazine.com/omega-xl.html
Q. Can allergies cause body aches?
A. Rarely do people associate joint pain with allergies. The truth however is that when allergies cause inflammation, joint pains are inevitable. Well, let’s first try to understand what allergies are .The Meaning of Allergies..https://www.jointhealthmagazine.com/how-is-joint-pain-tied-to-allergies.html
Q. What causes pain in the finger joints?
A. Imagine your fingers aching every time you use them. That could be awful. You cannot push a key on your laptop, complete a message on your Android phone, hit those guitar chords, thoroughly and thoroughly clean your body or the plate you used last night..https://www.jointhealthmagazine.com/finger-joint-pain.html
Q. What is in vital 3?
A. Vital 3 is a natural joint supplement that is sold and marketed to promote healthy joint muscles and at the same time to promote joint comfort and improve joint lubrication. As a long term joint care ingredient, this product is touted to work within the first six weeks..https://www.jointhealthmagazine.com/vital-3.html
What is Joint Effusion?
Every single one of us has fluid in our joints. It’s our body’s way of lubricating your joints so you can move around easily. However, Joint Effusion is when there occurs too much fluid builds up in the joints.
Joint Effusion can be caused by a number of different things. The cause of Joint Effusion impacts how your doctor will treat it so bear that in mind when you make your appointment.
What Causes Joint Effusion?

Joint Effusion can be caused by a number of reasons:
- Overusing the joint and causing repetitive injury from sports or household tasks.
- Tearing ligaments or cartilage
- Bacterial infection within the joint
- Burstitis (where the Bursa Sac fills with too much fluid).
- Breaking a bone
- Gout or pseudogout
- Cysts or tumors in the joint
- Rheumatoid Arthritis and/or Osteoarthritis
What are the Symptoms of Joint Effusion?

Depending on the cause of your Joint Effusion, you will likely experience different symptoms. For example, if you suffer from Osteoarthritis you’ll likely feel pain when your knee takes your weight.
Going from sitting to standing for example, and you’ll find that the pain goes away with relaxation.
If you have Joint Effusion from an injury, you’ll find there may be bruising and the pain may be too much to bare when standing. You’ll likely not be able to stand or walk at all.
Regardless of the cause of your Joint Effusion, you’ll probably notice that your knee becomes swollen. It may become larger than your other knee.
It may become difficult to bend your knee and you may notice Redness, heat and other signs of inflammation.
If Joint Effusion is left untreated, in severe cases you could contract an infection in the joints. Make sure you see a doctor ASAP if you get any of these symptoms.
Are you at Risk of Joint Effusion?

In reality, everyone is at risk of Joint Effusion. Anyone can put their knee joint under stress and cause Joint Effusion. However some are more at risk than others. These high-risk groups include:
- Older people – Your risk grows as you get older.
- People who regularly play sports that put stress on your joints such as Soccer, Basketball and Wrestling.
- People who work jobs that include a lot of kneeling such as roof layers, gardeners, carpet fitters etc.
- People who are overweight or obese – Carrying extra weight puts more stress on your joints.
- People with Arthritis and other health conditions that affect joints.
When do you need to see a Doctor?
Regular knee pain will go away after you’ve spent some time resting, applying ice and keeping the knee elevated. But how do you know when the pain is no longer normal and you should see a doctor?
- You know you’ve sustained a serious injury to your knee.
- You can’t bend your knee without pain.
- You can’t stand or walk for more than a few minutes without extreme pain.
- Your knee is warm, red and significantly larger than the other.
- If the tenderness and pain in your knee does not go after a few days.
How is Joint Effusion Diagnosed?
How is will your doctor diagnose you with Joint Effusion? Well, first of all, your doctor will take a look at your medical history.
They will have a look for any previous knee or joint conditions, including arthritis. It would also be a wise idea to share with your doctor if you have hobbies or a job that puts stress on your joints.
Your doctor will do a physical exam first. They will check your knee and test your range of motion. If the diagnosis is unclear, a fluid sample will be taken from your knee.
The sample is taken with a long, fine needle that is inserted into the joint space and the fluid will be withdrawn.
The extracted fluid will be tested for a number of things including certain bacteria that causes infection and crystals, protein and glucose that could indicate Gout.
The fluid will also be tested for blood cells that may indicate injury to the knee. The removal of fluid from the knee can often help with the pressure and pain that is caused by it.
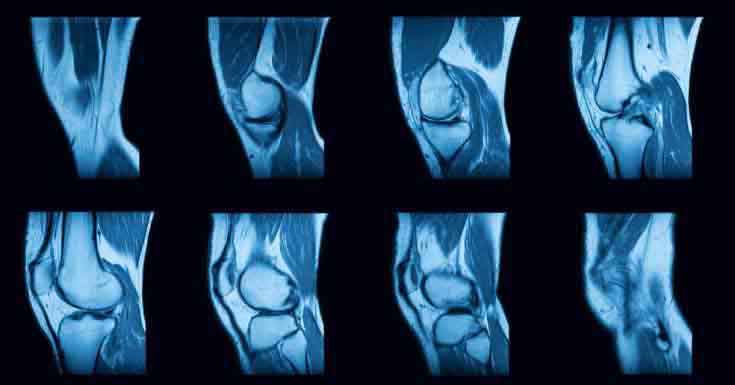
Lastly, your doctor may send you off for an imaging test. You could be sent for an MRI, CT Scan, Ultrasound or X-ray to help determine the cause.
How is Joint Effusion Treated?

The treatment will heavily rely on the results of your diagnosis. For example, depending on what the results of the fluid tests are. Your treatment could be any one of the following:
- Antibiotics for any infection
- Anti-Inflammatories and other pain medication.
- Oral Corticosteroids
- Corticosteroids that are injected directly into the joint.
- Joint aspiration to relieve pressure in the joint.
- Physiotherapy to build the strength of the supportive muscles and improve flexibility.
- Arthroscopy
If your knee doesn’t respond well to treatment, removal of the Bursa Sack may be needed or even knee replacement surgery for severe cases.
Conclusion
Joint Effusion is a pretty serious condition that can be caused by a number of different things. The key thing to take away from this is that you need to be protecting your joints. Especially if you do anything strenuous for work or hobbies such as gardening or sports.
Make sure that you take special care to protect your joints. Invest in a knee brace and try to maintain a healthy weight to avoid putting extra stress on your knees. And go to your doctor straight away if you notice any of the symptoms above.
Feature Image- Shutterstock.com
In- Post Image- Shutterstock.com







 This article changed my life!
This article changed my life! This article was informative.
This article was informative. I have a medical question.
I have a medical question.
 This article contains incorrect information.
This article contains incorrect information. This article doesn’t have the information I’m looking for.
This article doesn’t have the information I’m looking for.