The shoulder joint is the most mobile joint in the body, making it more susceptible to injuries and instabilities. The whole joint is encapsulated making its soft tissue structures such as ligaments, tendons, muscles and bursae closely packed together. If one structure becomes damaged, the other structures will follow.
What is Bursitis?
Bursitis is the inflammation of the bursa. Bursa, or bursae in the plural, is a fluid-filled sac that serves as a cushion. It works as a gliding surface that aids to reduce the friction in between the tissues of the body. Our body comprises 160 bursae mostly located near the tendons attached to the large joints such as the shoulders, elbows, hips and knees.
What is Shoulder Bursitis?
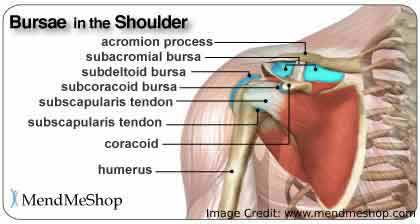
Shoulder bursitis is usually an inflamed bursa in the shoulder joint. But it can also be caused by injury, stress or inflammation from the rheumatic condition, or rarely caused by infection. There are three major bursae in the shoulder: subacromial bursa, subdeltoid bursa and the subscapular bursa.
The subacromial bursae are the most commonly inflamed among the three. This is usually due to impingement of the bursa between the rotator cuff tendons and the acromion process.
The acromion process forms the bony outer and superior part of the shoulder. Attached in between the acromion and the shoulder joint (or glenohumeral joint) are the rotator cuff muscles. These muscles are responsible for most of the range of motion available for the shoulder joint.
The subacromial bursa serves as a lubricating agent, providing cushion and reduces the rubbing between the bony acromion and the muscle tendons. Once irritated, the bursae thickens and causes pain with swelling.
Insult to the shoulder joint may cause bursitis. Repetitive shoulder movements with high-risk activities such as skiing, throwing and pitching increase the risks of bursitis. Pain most likely intensifies after prolonged and repetitive shoulder movements.
Overuse type of injuries is usually associated with tendonitis or the inflammation of rotator cuff muscle tendons and impingement in which structures around the joint rubs with the bony surfaces. High impact force or trauma on the shoulder can also lead to an inflamed bursa.
What are the Symptoms of Shoulder Bursitis?
The most common symptom of shoulder bursitis is a pain. Usually, the pain is easily localized accompanied by swelling, tenderness and painful shoulder arc movements. The onset of the symptoms is usually gradual for over weeks and months.
A person with shoulder bursitis may find it difficult to raise the arms above the head especially when getting dressed or put some pressure on the affected shoulder, as it would induce pain.
Pain is usually made worse when lying on the affected side and during overhead shoulder movements especially the 60°-90° shoulder range. It is usually characterized as a “pinching” pain felt especially during physical tests. The pain may radiate from the outer part of the shoulder to the outside of the arm, almost pass the elbows.
As the condition persists without proper treatment, muscle weakness of the affected shoulder may result. People with shoulder bursitis caused by infection will experience fever, redness and warmth.
How to Diagnose Shoulder Bursitis?

Obtaining medical history is important. Normally, the doctor will be asking about the quality and location of pain felt, details about the onset of the symptoms, and if you have a physically active lifestyle. Physical tests and examinations will follow.
Active and passive shoulder movements will be assessed and your shoulders will be checked for any deformity or tenderness. The doctor will examine the patient’s joint, noting any swelling, tenderness or points of pain.
To rule out other possible diagnoses or abnormalities associated with shoulder bursitis, diagnostic procedures are usually done. This includes:
- X-ray Uses an electromagnetic radiation to produce two-dimensional images of tissues, bones and organs. X-ray testing can detect calcifications in the bursa indicating its severity. Usually, calcifications are formed when the bursitis is already chronic.
- Magnetic Resonance Imaging (MRI) and ultrasound Produces detailed pictures of bones, soft tissues, organs and all other internal structures. It provides a better view to detect abnormalities of structures such as thickened or swollen bursa.
- Anesthetic Injection To identify whether the diagnosis is an impingement syndrome or bursitis, an anaesthetic called lidocaine hydrochloride will be injected under the acromion process. If symptoms are relieved after the administration of anaesthetic, impingement syndrome is the cause.
- Aspiration and Lab Tests Septic bursitis is a serious, life-threatening condition. The infection may travel through the bloodstream if left unattended. Aspiration is a process of obtaining fluid from the bursa with a needle and syringe.
What is the Prognosis of Shoulder Bursitis?

The prognosis of shoulder bursitis largely depends on the severity of the injury. Full recovery of structures affected is expected for acute cases. However, chronic bursitis is usually associated with scarring, around the joint (also known as calcific bursitis or frozen shoulder syndrome). This would require long-term rehabilitation.
Calcific Bursitis is the presence of bone growth within the bursa. This results in immobility or limited available range of motion and pain. In this case, corticosteroid injections are the first line of management to decrease the pain. After about one week, the patient will be cleared for physiotherapy to address biomechanical issues.
How to Prevent Shoulder Bursitis?
Prevention is definitely better and cheaper than cure. These are the things that you should keep in mind to lessen or prevent the risks of having shoulder bursitis:
- Warm up and stretching your muscles are necessary before you start exercises or any physical activity with repetitive movements
- Avoid activities that require repetitive overhead movements for long periods of time
- Take breaks when doing a lot of repetitive tasks
- Maintain good posture and correct body positioning
- Gradually increase levels of activity especially during exercise
- Respect pain. If you felt that certain movements cause pain, it’s best to stop and take some rest
What are the Treatment for Shoulder Bursitis?

Treatment of Shoulder Bursitis depends on the underlying cause and its severity. The line of management will depend on your age, activity level and general health.
Since not all cases require surgical intervention, most doctors recommend the term RICE.
R for rest, I for Ice, C for Compression and E for Elevation. This is a recommended initial strategy to lessen the symptoms of bursitis. Along with this, Non-steroidal Anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, naproxen and cox-2 inhibitors are usually prescribed to minimize the pain and swelling.
Topical medications are also recommended and are applied directly to the skin over the affected joint. This may be the best choice for patients who experience side effects from oral medications.
A swollen bursa requires aspiration. This is the removal of fluid in the bursa with a needle and syringe. The fluid will then be analyzed in the laboratory. Also, corticosteroids are injected in the bursa to decrease inflammation.
Physical aids such as a cane, splint, brace or other supports will be recommended by the doctor to assist in positioning and optimally reduce stress on the joint.
Furthermore, infectious or septic shoulder bursitis (usually uncommon), requires more thorough and aggressive treatment. Analysis of bursa fluid is required to help with identifying the microbes causing the infection.
Antibiotic therapy is commonly the line of treatment which is usually administered intravenously. Prescription of antibiotics will depend on the type of bacteria causing the infection, commonly Staphylococcus aureus.
When non-surgical treatment does not relieve pain, surgery is recommended. The removal of swollen or infected bursa sac (called bursectomy) will be done. After removing the injured bursa, a new one will form in its place. Some doctors usually perform arthroscopic bursectomies.
Once the wound is healed, normal shoulder functions will ensue. Consequently, the doctor may order physical therapy to help strengthen impaired muscles in the area and improve mobility. If the bursitis is caused by damage to the rotator cuff tendons, tendon repair will be done.
Subacromial decompression (acromioplasty) is another option, in which part of the acromion is removed to give enough space for the soft tissues inside the shoulder complex. However, research says that bursectomy alone is less invasive and easier to recover from.
The rehabilitation phase will primarily focus on joint mobilizations, shoulder muscle stretches, light passive and active exercises to help regain range of motion. Researchers have learned that rotator cuff muscle strengthening exercises will aid in restoring the stability of the shoulder joint.
However, healing of injured muscle tissues should first take place before providing load or anti-gravity exercises. Unfortunately, once a thorough rehabilitation program is not completed and the patient will return immediately back to work or daily activities, the bursitis is likely to recur.
To prevent recurrence, consult your physiotherapist or occupational therapist about the proper exercises including the correct positioning and modifications necessary.
Who Should I Call for Treatment?

In most cases, a general medicine physician including general practitioners, family medicine doctors and internists can treat bursitis. You may also go to your orthopaedic surgeon, rheumatologist, and sports medicine specialist.
For rehabilitation, physical therapists and occupational therapists are usually ordered by the physician to regain normal functions to fulfil your day-to-day activities.
Read Next: Shoulder Arthritis: Types of Arthritis That Affect the Shoulder
Conclusion
Shoulder bursitis is usually caused by an overuse injury. The prognosis depends on a lot of factors determined by series of tests and examinations by your doctor. Good prognosis relies on a carefully planned rehabilitation program that is critical of each progression so that it will not lead to frustration and recursion of injury.
Preventing risks of having bursitis is important to protect other joints as well.
For more information and questions about your shoulder or subacromial bursitis, you may contact your physician or physiotherapist.
Feature Image: Shutterstock.com
In Post Image: www.mendmeshop.com, Shutterstock.com







 This article changed my life!
This article changed my life! This article was informative.
This article was informative. I have a medical question.
I have a medical question.
 This article contains incorrect information.
This article contains incorrect information. This article doesn’t have the information I’m looking for.
This article doesn’t have the information I’m looking for.